Predicting Chronic Disease Risk with Data

Treating chronic diseases is one of the largest costs to the health care industry. But many chronic diseases have early warning signs. And just as doctors can spot these warning signs in individual patients, public health workers can spot them in entire populations, using easily available data.
States and providers are using predictive analytics to determine which patients are at a higher risk for disease, and then creating interventions before the problems arise. These analytics involve an individual’s medical and family history, as well as socio-economic data like employment, education, and physical environment.
These socio-economic indicators are available from federal data agencies like the Census. For example, the Census’s American Community Survey (ACS) has data on education and poverty, which we can look at at the census tract level (often smaller than a neighborhood). The Centers for Disease Control and Prevention’s (CDC) Behavioral Risk Factor Surveillance System (BRFSS) has data on what types of people are susceptible to different conditions; PolicyMap combined that data with ACS data to create census tract level maps of health risks.
In Philadelphia, there are census tracts where over 25% of the population does not have at least a 9th grade education, lives in poverty, and currently smokes.
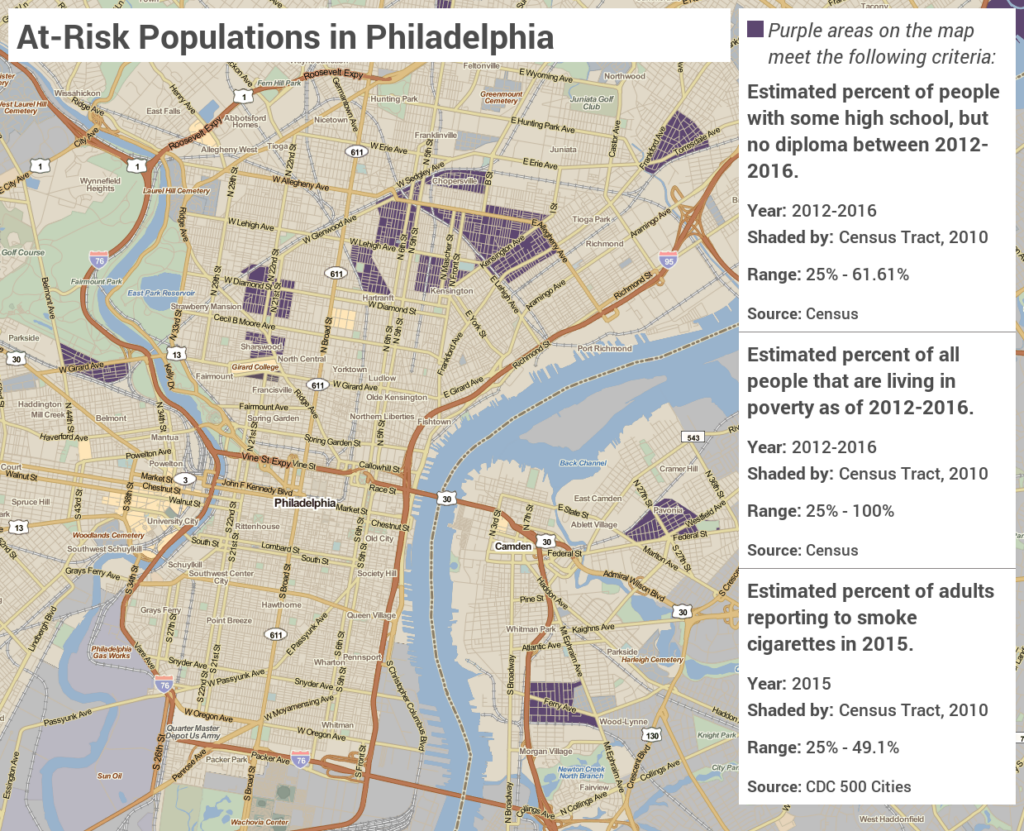
These conditions pinpoint areas susceptible to higher rates of chronic disease where health care providers should look to target interventions, such as anti-vaping campaigns or smoking cessation incentives as successfully done in Massachusetts.
In Massachusetts, data showed that a relatively high proportion of low-income people insured by Medicaid were smokers. After the state funded tobacco cessation benefits for Medicaid recipients, in-patient admissions for cardiovascular conditions were reduced. Using data from the Medical Expenditure Panel Survey and from the Behavioral Risk Factor Surveillance Survey (BRFSS), researchers determined that by funding the cessation program, the state saved about $183 per participant, and every $1 spent in benefits was associated with $3.12 in medical savings.
This post was adapted from our recent white paper, “Do Our Zip Codes Need to Determine Our Health?” You can download the complete paper here.