Can Telemedicine Help Us All?

Data
Computer and Internet Access
Source
Census
Find on PolicyMap
- Health
- COVID-19
- Computer and Internet Access
- COVID-19
With growing pressure on the health care system due to COVID-19, health officials are increasingly turning to “telemedicine” for routine visits and for evaluating patients with and without COVID-19 symptoms.
Telemedicine allows doctors’ offices to address patient needs while reducing the spread of COVID-19. It also allows for “medical distancing,” keeping healthcare providers away from sick patients to reduce transmission. Providers can then determine whether a patient with COVID-19 symptoms requires medical care or can self-isolate and recover at home.
For this to work, households need to have an internet connection and a computer, tablet or a smart phone so that a doctor can visually examine a patient. Healthcare providers need both the equipment to conduct the online visit and a doctor, nurse practitioner, or nurse to perform the virtual exam. While many are on the front line physically helping in hospitals, doctors who are at greater risk of serious infection from the virus are making up the telemedicine force. Older doctors, doctors with chronic conditions and, yes, doctors who are infected and quarantined are performing these telemedicine appointments.
Doing this on a large scale requires that both healthcare providers and patients have the needed “telecommunications services, information services and devices necessary to enable the provision of telehealth services during this emergency period,” as described by the Federal Communications Commission.
Federal agencies are taking steps to help:
- Medicare restrictions which required that patients live in a medically underserved area in order to receive telehealth services have been waived during this emergency.
- Centers for Medicare and Medicaid (CMS) is also waiving the requirement that the practitioner use a HIPAA-compliant platform for the telehealth service. Telehealth must be delivered in real-time, using a platform that provides the provider the ability to both see and hear the patient, but FaceTime and Skype, both of which can be accessed on a smartphone, are acceptable.
- The recently passed Relief Act provides $180 million to carry out telehealth, with specific emphasis on rural areas where getting to a doctor’s office is difficult. In places with poor access to health facilities, telehealth is seen as a necessity in evaluating patients.
- Federally Qualified Health Centers (FQHC) and Rural Health Clinics (RHC)—sites which were previously prohibited from providing telehealth services—can now do so during this emergency.
Because an internet connection and access to a computer, tablet or smart phone are requirements for this to work, however, there are households—poorer urban households and rural communities in particular—which are going to need more strategic assistance in order to access this needed service.
Looking at these two factors across the US, we can see places (census tracts) where over one-third of households do not have access to any internet service or where over one-third do not have access to a computer or smartphone. These are the places where significant numbers of households lack at least one of the basic requirements to do telemedicine.
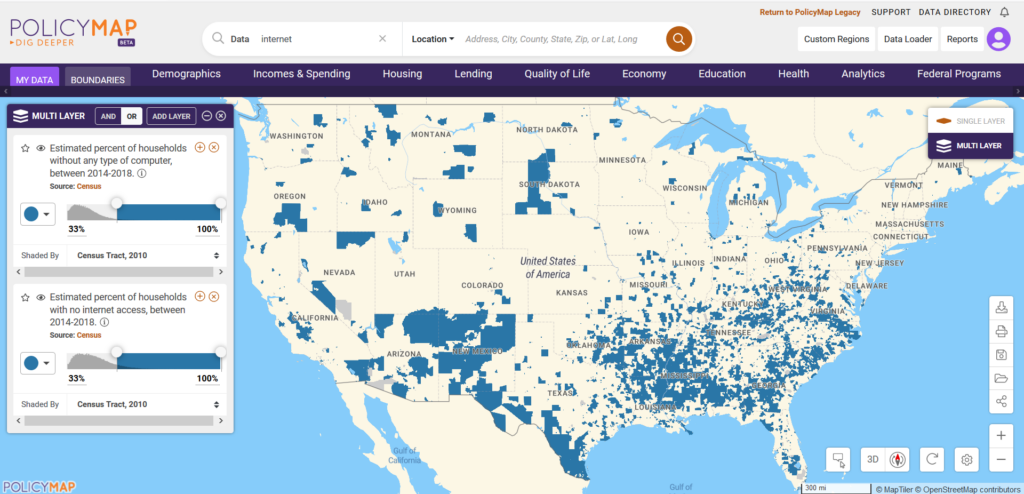
Learn how to do this on PolicyMap now.
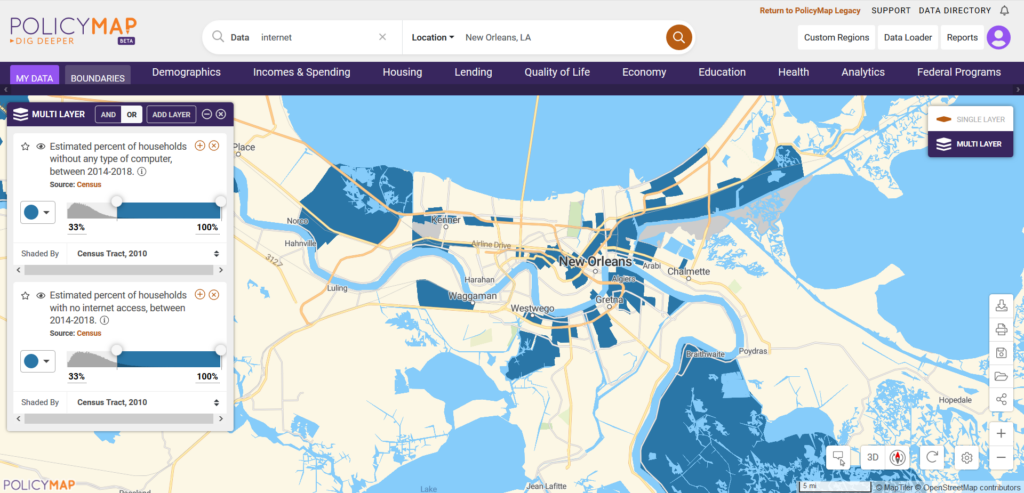
If we take a closer look at New Orleans, a city expected to be severely impacted by this virus, we can see the specific census tracts within the City where providing telemedicine will be most problematic. These census tracts are home to almost 60,000 households and over 150,000 people. One third will likely not be able to access telemedicine opportunities. Using this kind of data now can help cities and rural areas strategically plan for the weeks ahead.
As healthcare providers face overwhelming demand for their services, telehealth is a means to save time and money, but more importantly, lives during this crisis. Without planning for interventions to ensure service to those without connectivity, however, we run the risk of denying opportunities for critical resources among those in need.
On April 8, the Center for Technology Innovation at Brookings will host a webinar to discuss what federal and local leaders are doing now to mitigate these kinds of challenges. Learn more and register for their webinar.