Opioid Data Can Be Confusing – Here’s Why

As we added new opioid-related data to PolicyMap, we noticed in the course of our validation that in Philadelphia (where we’re based), the CDC reported only 27 total deaths due to opioid overdose in 2016 (the most recent year of data available). This number seemed surprisingly low.
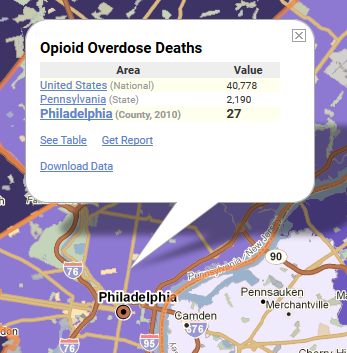
By contrast, the City of Philadelphia reported over 725 deaths due to opioids in 2016, 26 times more than the CDC reported. A recent Pew study likewise lists Philadelphia as having the second highest death rate from opioid overdoses in 2016 among counties with populations over one million. In a city known for an open air drug market, clearly we were missing something in the CDC opioid overdose death data.
According to the CDC, more than 350,000 people died nationwide from drug overdoses involving an opioid between 1999 and 2016. However, a recent study published in Public Health Reports suggests that these CDC numbers likely under-report opioid-related overdose deaths by 20 to 35 percent. The study finds as many as 70,000 opioid overdose deaths were unreported or misclassified between 1999 and 2015, largely due to inaccurately completed death certificates.
Inaccurately completed death certificates are likely the root cause of the discrepancies with the CDC-reported opioid poisoning. The CDC collects data from state health departments, which collect data from county coroners and medical examiners. Any differences in how death certificates are completed at the local or state level will trickle up to the CDC data.
We rely on data to help us understand and explain the story of what is causing the spike in opioid deaths, so what do we make of this sort of suspect data? What’s causing it, and how do we deal with it?
Understanding Death Certificates
Understanding irregularities in the CDC data requires an understanding of death certificates, the source of the CDC data.
In order to capture the full story of what contributed to a person’s death, there are typically several causes of death listed on a death certificate. The immediate cause of death refers to what actively caused a death, such as a heart stopping or neural brain death. Also included are other preceding causes of death and the original underlying cause of death.
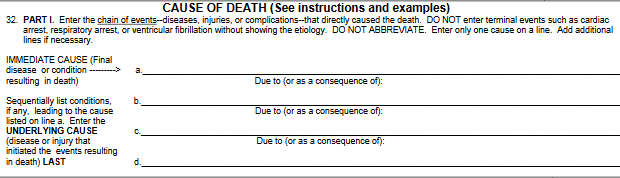
Drug overdose is never the immediate cause of death. Immediate death is more typically the result of something like cardiac arrest. Because of this, death certificates for opioid overdose should list several other preceding causes of death.
Taking opioids causes shallow breathing, also called respiratory depression, which in itself is not usually fatal. However, in large doses this symptom can become fatal by causing a complete lack of breathing (anoxia), which leads to heart stoppage and brain damage if not immediately treated.
Thus, a death certificate filled out for an opioid overdose would likely list cardiac arrest as the immediate cause of death, with respiratory depression and anoxia as preceding causes, and a specific type or combination of opioids as the underlying cause.
The CDC recommends that the final underlying cause of death should be specific enough that “it does not leave any doubt as to why it developed.” However, many death certificates arrive at state health departments without listing which drug or drugs contributed to the death.
Missing Data in Death Certificates
A host of reasons contribute to this lack of detailed information on death certificates.
The Council of State and Territorial Epidemiologists analyzed the practice of using death certificates to study drug poisoning. They found that the circumstances surrounding overdose deaths are typically complicated, and toxicology testing to determine specific drug types can take a long time to return results. State regulations usually require timely reporting of deaths. This leads many certifiers to submit the certification without including specific underlying causes of death. As many as 75% of drug overdose death data lack a specific drug reported on the death certificate.
Toxicology reports are also expensive and can strain local budgets, especially in places that are experiencing high rates of drug overdose deaths. This may be an additional reason why specific drugs are not listed on death certificates.
Often, coroners and medical examiners leave off these details because of a lack of understanding about the importance of including drug details for epidemiological data, or confusion over how to report poisonings, especially when multiple drugs are involved. For instance, some death certificates list vague causes that do not include specific drugs, such as “acute overdose” and “multiple drug intoxication,” which are not standard causes of death. A lack of oversight in many states does little to address these practices.
While one might expect that someone filling out a death certificate would have medical expertise, this is not always the case. Because drug overdose deaths rarely take place in a hospital, most of these death certificates are filled out by medical examiners and coroners rather than physicians.
While most medical examiner positions require some medical background, many coroner positions are appointed or elected and rarely require any previous medical experience or qualification. Counties with smaller populations typically have a part-time coroner. This coroner often lacks appropriate training and facilities, and may even face conflicts of interest by also holding a position as a funeral director, prosecutor, or sheriff.
The consequences of this lack of medical expertise and limited resources for coroners are substantial. One study found that among overdose deaths, states with centralized state medical examiner systems were significantly more likely to list specific drug types on death certificates (92%) as compared with states with decentralized county coroner systems, where only 62% of overdose death certificates listed drug types.
In short, in some cases, certifiers are underqualified and under time pressure, and lack sufficient oversight, resources, funding for toxicology tests, and understanding of the importance of including drug details on death certificates. Fortunately, several states have recognized the need for a coordinated effort to collect better information and have been able to reduce the number of unreported opioid overdose deaths over the past few years.
For more information about this issue and some of the efforts in place to try to combat it, see these stories on Indiana, Kentucky, and Ohio.
For more information on the challenges of leaving death investigations to coroners, visit this NPR investigation.
Working Around the Limitations
If up to 20-30% of opioid overdose deaths are missing from the CDC’s opioid overdose data, where do we go about finding these missing values?
To begin, it helps to understand how different drug types get coded. If one or more specific opioid types is listed on a death certificate, it gets coded with one of the following ICD 10 codes: heroin (T40.1), natural and semisynthetic opioids other than heroin (T40.2), methadone (T40.3), and synthetic opioids other than methadone (T40.4). The category of data for “all opioid overdoses” includes all these categories (T40.1, T40.2, T40.3, and T40.4). Opium (T40.0) is not included since fewer than 10 people are reported each year as having died from opium overdose nationwide.
When a death certificate includes a reference to opioids, but fails to list a specific type, it usually gets categorized under “unspecified narcotics” (T40.6).
The underlying cause of drug overdose deaths rarely gets classified as “unspecified narcotics,” but it is a good place to check when searching for missing opioid overdose records. Keep in mind, however, that because the legal definition of narcotics in the U.S. includes cocaine and cocaine derivatives in addition to opioids, this unspecified narcotics category may include deaths due to cocaine substances.
Most missing opioid overdose death records lack enough detail to end up categorized even in the broadest narcotics category, and therefore end up listed under “unspecified drugs” (T50.9).
As the map shows, the number of unspecified drug overdose records varies dramatically between states. It turns out that Pennsylvania has one of the highest rates of unclassified drug overdose records. In the previously mentioned study on underreporting of opioid deaths, Pennsylvania was among five states (also including Alabama, Indiana, Louisiana, and Mississippi) where more than 35% of unintentional overdose deaths were mis-coded as unspecified drugs.
Looking at Philadelphia, we can see that the missing 700 or so opioid overdose records likely ended up in this category.
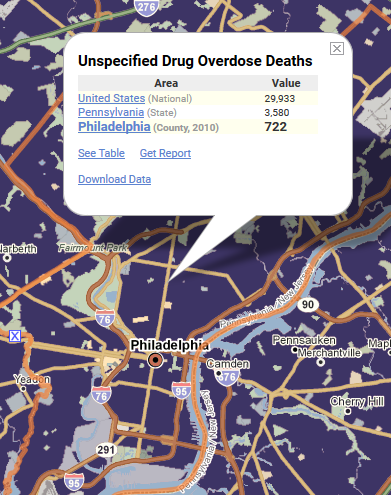
While a 2013 study reported that overall, approximately 25% of overdose deaths failed to list a specific drug type, a study by the National Drug Early Warning System found that in Philadelphia, more than 80% of drug overdose poisonings failed to list a specific drug type.
Not all deaths included in this unspecified drug category necessarily include opioids, but it is likely that in geographies with unexpectedly low values for opioid-related deaths, the missing opioid overdose deaths are ending up in this category.
For more information on how death certificates get coded with ICD codes and an analysis of different states, see this Public Health Reports study.
So what should you do when looking at the data? Start by looking at opioid-related deaths. If that number is not available, or seems too low, then also take a look at deaths from unspecified narcotics and deaths from unspecified drugs.
Clear and accurate information on the scope of opioid overdoses is essential to addressing the crisis. Local practices for filling out death certificates are improving, but in the meantime, it’s important to understand the limitations of the data, and how to use it despite those limitations.