Understanding Healthcare Access Through the Compendium of U.S. Health Systems

Measuring and evaluating access to healthcare has long been a challenge for researchers and policymakers. One reason is the complexity of relationships between healthcare facilities and how those relationships shape the availability, quality, and delivery of care. In many regions, outpatient facilities, hospitals, and physician practices operate as part of larger networks known as health systems. These systems influence where facilities are located, how patients navigate care, and the overall patient experience.
The Compendium of U.S. Health Systems
As part of its initiative to study how health care systems promote evidence-based practices in delivering care, the Agency for Healthcare Research and Quality (AHRQ) created the Compendium of U.S. Health Systems, a consolidated list of health systems across the United States and the facilities associated with them.
AHRQ defines a health system as:
“A health system includes at least one hospital and at least one group of physicians that provides comprehensive care (including primary and specialty care) who are connected with each other and with the hospital through common ownership or joint management.”
To qualify as a health system, an organization must include:
- At least one non-federal acute care hospital
- At least 50 physicians
- At least 10 primary care physicians
The Compendium contains four primary facility files—hospitals, outpatient sites, nursing homes, and home health care organizations—which are linked through a system-level file identifying each health system and its associated facilities.
As with other datasets on PolicyMap, each facility type in the Compendium is published with filters to help users tailor their analysis. The outpatient sites layer includes a specialty filter that captures both traditional medical specialties—such as dermatology, primary care, and neurology—as well as treatment-focused facilities like wound care centers and dialysis clinics. Hospitals can be filtered by ownership structure, insurance plan offerings, and hospital type, allowing users to quickly identify the kinds of services and systems present in a community.
Connecting Facilities, Systems, and Communities with PolicyMap
With this release, researchers, healthcare organizations, and other stakeholders can map and analyze the locations of facilities that participate in health systems across the United States. When combined with other demographic or health-related datasets available on PolicyMap, the Compendium becomes a powerful tool for exploring healthcare access, quality, and equity.
Visualizing Healthcare Access in Washington, D.C.
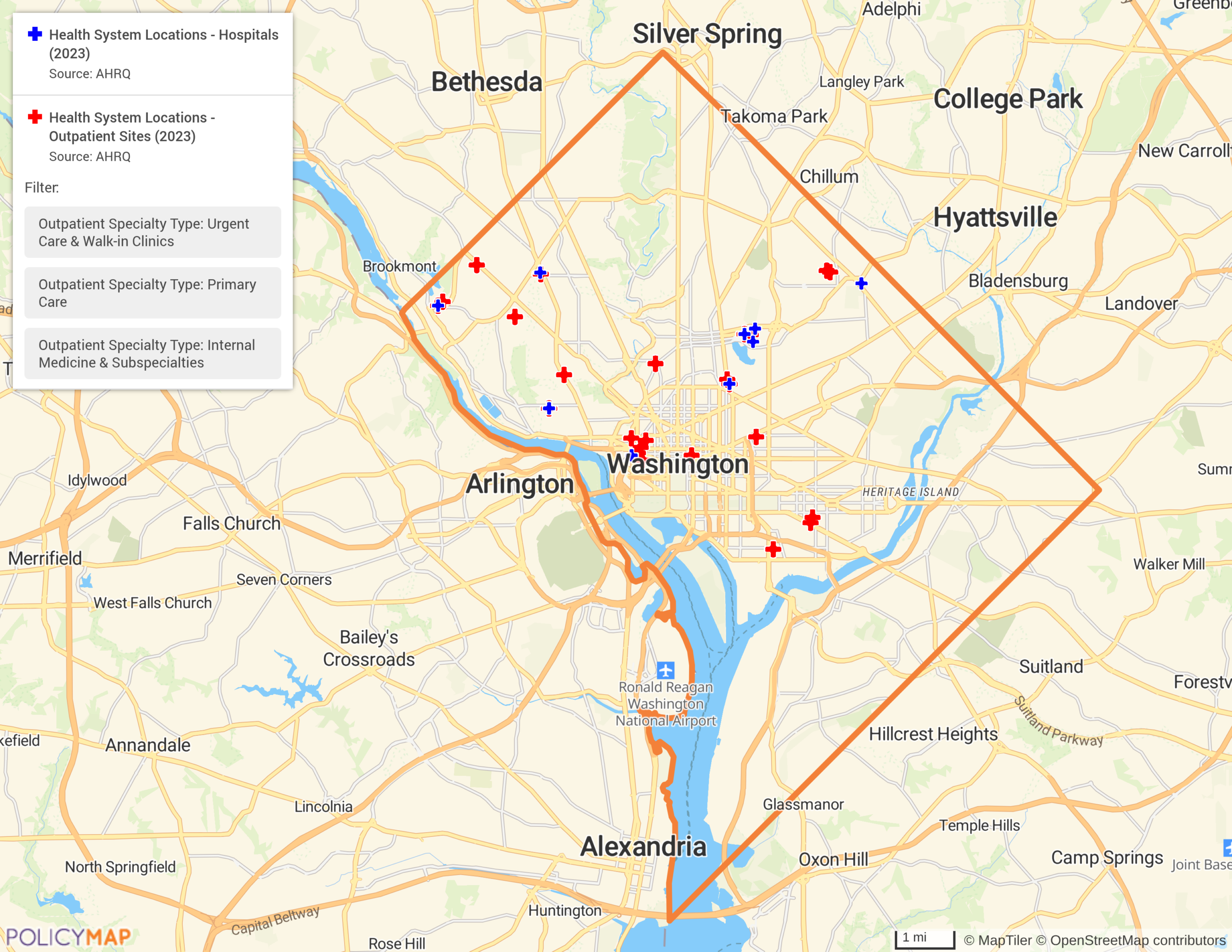
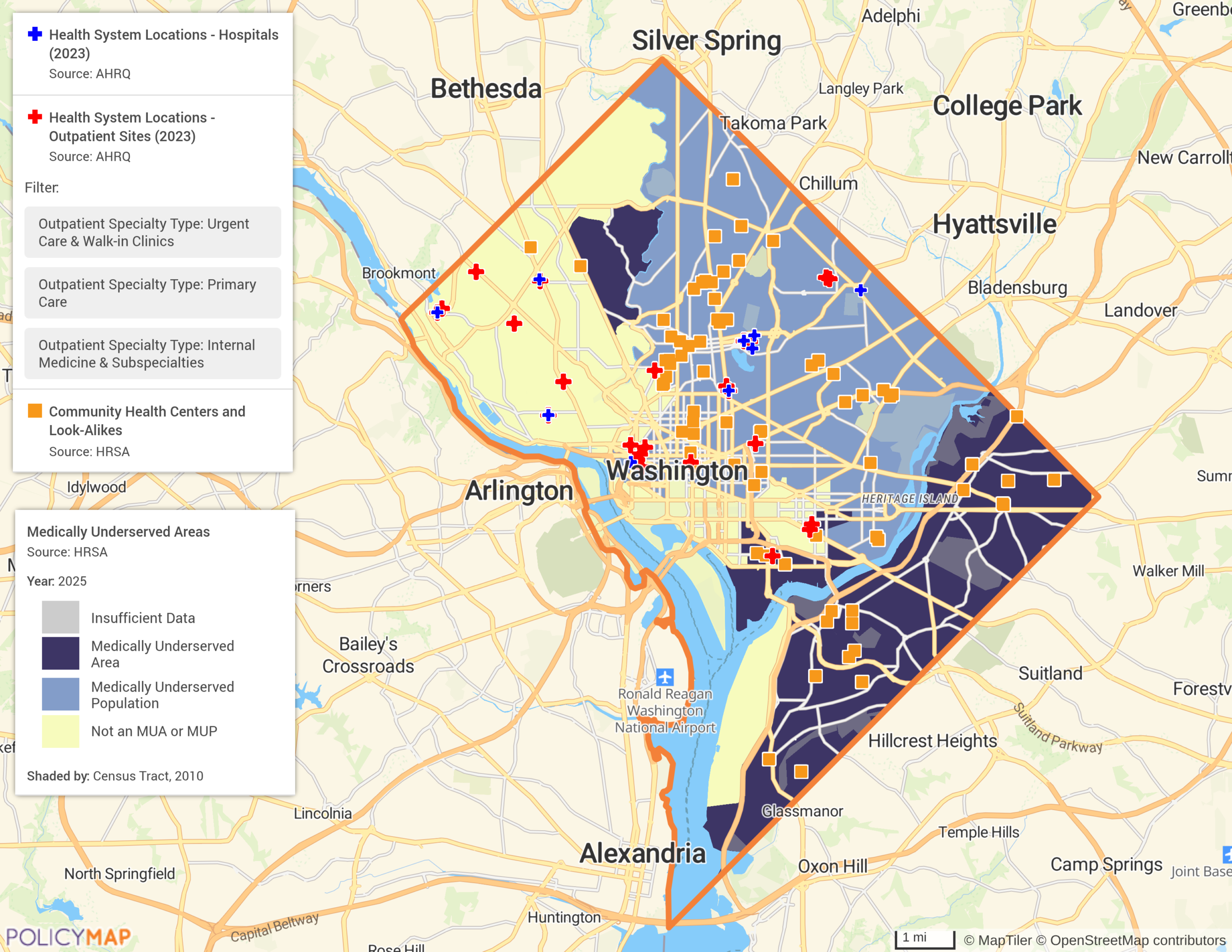
Washington, D.C. is home to multiple private and university-affiliated health systems. Mapping Compendium data reveals important disparities in where system-affiliated care is available.
In the southeast region of D.C. across the Anacostia River—a historically lower-income and underserved area—there are no health system-affiliated hospitals, walk-inclinics, internal medicine, or primary care practices. By contrast, neighborhoods in other areas of D.C. have ready access to both hospitals and providers.
When combined with HRSA’s Medically Underserved Areas (MUA) layer and Community Health Center locations, the picture becomes even clearer. Most of the southeast region is designated as medically underserved, reflecting limited provider availability, higher poverty levels, higher infant mortality, and larger elderly populations. Residents of this area primarily depend on community health centers for healthcare—facilities that often rely on grant funding and may have more limited access to providers, technologies, and resources than larger health systems. Layering data from these different sources enables organizations to build a more complete picture of health disparities—one that single datasets cannot create alone.
Identifying Provider Shortages in Rural Communities
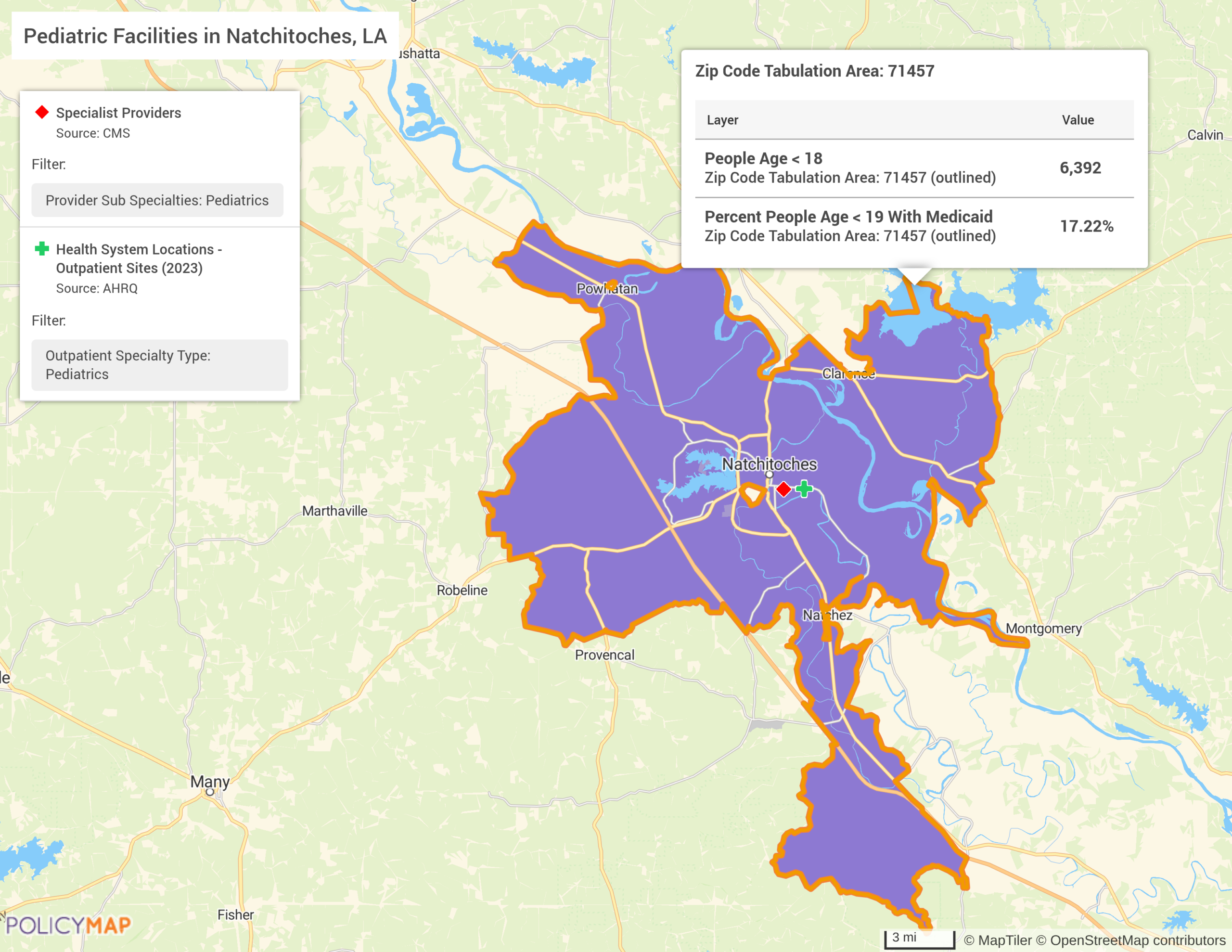
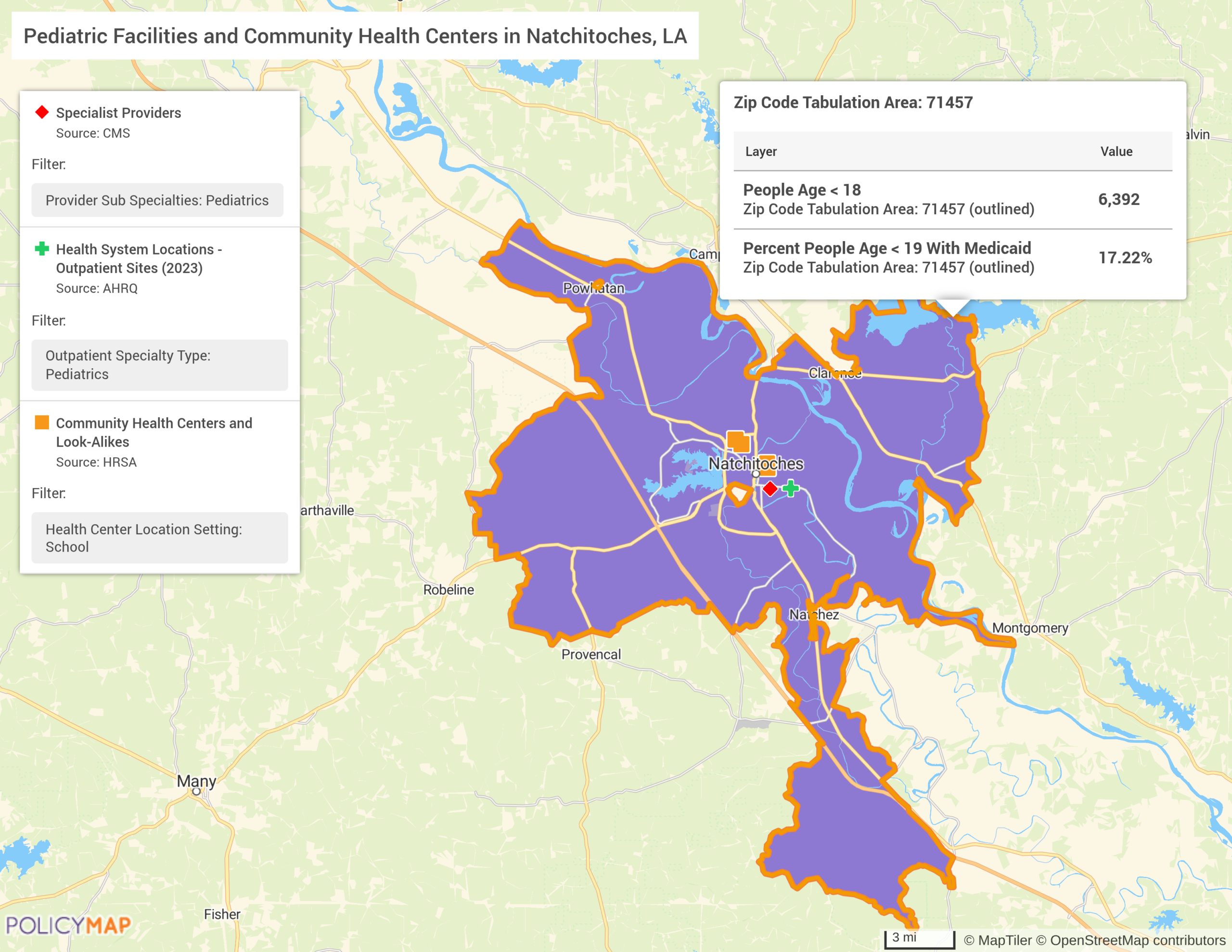
Healthcare access challenges are often even more pronounced in rural areas. In Natchitoches, Louisiana, for example, Census data show that among the more than 6,000 children in the community, 17% are enrolled in Medicaid. A health needs assessment completed by the Natchitoches Regional Medical Center in 2023 highlighted these issues, finding the second highest priority in the community was access to affordable healthcare and access to primary care providers and specialists. In focus groups, many residents expressed concerns over the lack of Medicaid-accepting providers and the ability to take their children to routine and wellness appointments.
Layering Compendium facility locations with CMS provider data reveals that only two pediatric facilities are serving the entire population. Data within the information bubble show that there are only three total pediatric providers across these two facilities—a ratio of roughly 1 provider per 2,000 children.
Adding in the same HRSA dataset shows that like D.C., Natchitoches heavily relies on community health centers to fill in the gaps. The community has five community health centers, three of which are based in schools. These school-based centers frequently provide care for children who otherwise struggle to access traditional medical providers.
Provider shortages like these can result in longer travel times, extended wait periods, and in some cases, delayed or forgone care. The Compendium gives users a clearer view of how the structure and distribution of health systems contribute to these access issues.
Explore Health Systems Data on PolicyMap
Interested in using the Compendium of U.S. Health Systems to better understand healthcare access in your community? Get in touch with our sales team to learn more about pricing and schedule a personalized demo tailored to your organization’s goals.