Mapping the Health Care Crisis in the American South
In an article from last weekend’s edition of the New York Times Magazine, author Suzy Hansen offers a harrowing view of the deteriorating health conditions spread across the American south. Hansen follows the work of three men – Dr. Aaron Shirley, James Miller, and Mohammad Shahbazi, respectively, a civil rights hero, a hospital business consultant, and a university professor – in their fight to redirect the failures of health care across the Mississippi Delta Region. Hansen’s article asks the question, “What can Mississippi learn from Iran?” by exploring the potential that mimicking Persian Health Houses, here in the U.S. might offer to under-insured and under-served residents in the Delta region. These service centers offered Iran’s rural villagers intermediary access to health services and advice without excessive costs. The article highlights HealthConnect, Dr. Shirley’s community health service that offers in-home care in addition to services operating out of local schools around Jackson, MS. The primary purpose of these services aims to reduce admissions and readmissions to area hospitals, by attending to rural community members with less access to regular care, and to encourage and facilitate preventive options. With the primary epidemic in the region being diabetes, hypertension, congestive heart failure, and asthma, many health issues are related to increased rates of obesity, and – as Shahbazi points out – poor diet and low-access to quality, healthful food. These three men started their Iranian-inspired project – hoping to set up 15 Health Houses – in order to show that they could affect health outcomes, while simultaneously reducing the costs of care.
The article notes a rise in other devastating statistics, which highlight disparities among both racial and geographic divisions – like that of infant mortality (for which the rate among black infants is more than twice that of white infants), and HIV/AIDS (for which the mortality rate is 64% higher among black populations in Mississippi than the nation’s average). For people like Shahbazi or Shirley, addressing these epidemics is as much about providing care as it is about understanding the social determinants of one’s health. It is important to understand how much can be learned from an in-home visit, with regard to a patient’s ability to manage his/her disease. Just as it is important to understand one’s geographic context, within areas that are remote, medically underserved, economically depressed, or void of healthful food options.
PolicyMap has a number of maps relevant to this topic. In our Health tab we have estimates for adult rates of diabetes and obesity. You can view by census tract, areas designated by Health and Human Services as Medically Underserved, areas designated by The Reinvestment Fund with Limited Supermarket Access, as well as rates of populations without health insurance. There is also point data (listed under the add sites function), of hospitals, health centers, and related health care provider information.
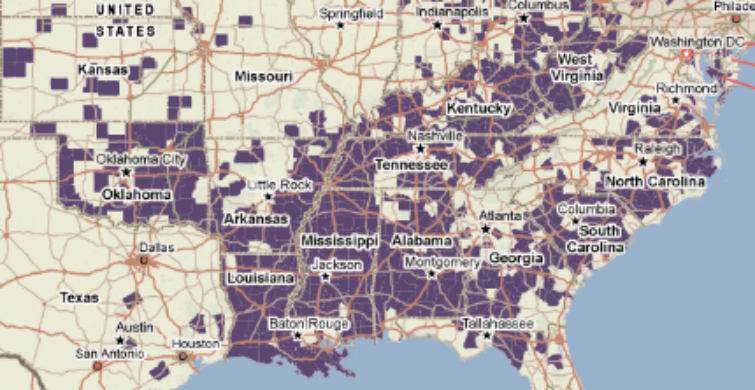
The following map can give you an idea of the types of information you can convey with these datasets.

Using the PolicyMap analytics tool, the map shows areas by county, where more than 25% of people, aged 18-64, who are living in poverty are uninsured (in 2009), more than 30% of the adult population is obese (as of 2008), and more than 10% of the adult population is diabetic (as of 2008). Nationwide, this map shows a shocking disparity of health conditions across the county, illustrating the grim reality of the current situation plaguing populations across the American south. What other relationships and correlations might be interesting to map? How can we use these maps to bring attention to the severity of the health care crisis? Let this serve as a starting point for exploring this critical topic.