New Data on Healthcare Associated Infections

Data
Hospitals: Quality of Care (Medicare Certified Hospitals)
Source
CMS & HRSA
Find on PolicyMap
- Health
- Health Facilities
- Hospitals
- Hospitals: Quality of Care (Medicare Certified Hospitals)
- Hospitals
- Health Facilities
We think of hospitals as places sick people go to get better. Unfortunately, there’s an inherent risk that patients might develop infections inside hospitals. Some of these infections are preventable if the hospital takes certain precautionary steps, like enforcing consistent hand-washing. Public data can help us see which hospitals are doing the best at preventing the Healthcare Associated Infections.
Last year, we introduced a dataset from the Centers for Medicare and Medicaid Services (CMS) that compares a variety of quality of care indicators across Medicare-certified hospitals. This data now includes a new indicator – Healthcare Associated Infections (HAI) – to deepen data users’ understanding of the quality of care that hospitals are providing to their patients. This information can be used by individuals in making informed decisions about their healthcare options, or help policymakers locate problematic facilities.
Click on a hospital below to see the HAI data (in the last tab):
The Newest Indicator
The HAI indicator evaluates each hospital across six measures:
- A central line-associated bloodstream infection occurs when bacteria enters the bloodstream through the central line (a tube place in a large vein that empties near the heart).
- A catheter-associated urinary tract infection occurs when bacteria enter the urinary tract through the urinary catheter and causes infection.
- Colon and abdominal hysterectomy surgical site infections occur when bacteria enter the body at the site of surgery and cause either a superficial infection of the skin, or a more serious infection of the underlying tissue, organs, or implanted material.
- MRSA is a type of antibiotic resistant bacteria and leads to many serious bloodstream infections, pneumonia, and other diseases.
- Clostridium difficile intestinal infections occur when the C. difficile bacteria – living in human feces – enter the body through the mouth or other mucous membranes, resulting in inflammation of the colon.
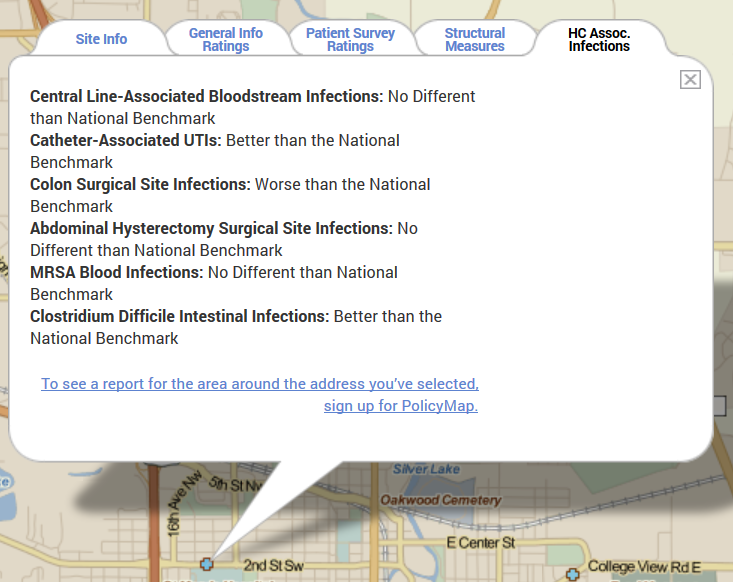
Each of these metrics are denoted as “no different than national benchmark”, “better than national benchmark”, “worse than national benchmark”, or “not available”. Below, the HAI information tab for the Mayo Clinic in Rochester, MN, one of the best hospitals in America.
HAIs’ Impact
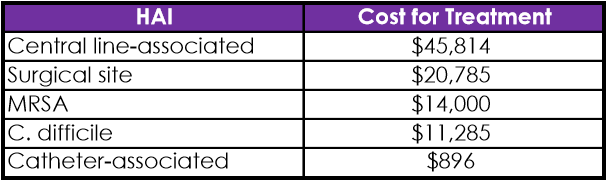
HAIs have a significant impact on the US healthcare system. At any given moment, one in 25 hospitalized patients (4%) are affected by an HAI. The CDC reports that two million patients require treatment for an HAI each year, of which nearly 100,000 die. Additionally, HAIs are expensive – the most expensive to treat is a central line-associated bloodstream infection, costing $45,814 per patient. Surgical site infections cost $20,785, MRSA $14,000, C. difficile infections $11,285, and catheter-associated urinary tract infections $896 to treat per patient.
Preventing HAIs
The kicker is that most HAIs are preventable; adhering to existing prevention practices would lead to an almost 70 percent reduction in some HAIs, and save the health care system between $25 and $31.5 billion each year.
The simplest approach to decreasing the number of HAIs is for healthcare professionals to wash their hands between patients. Though the effectiveness of hand washing has been known for decades, clinician compliance was low until recently. The most effective strategies for improving hand hygiene combine education, monitoring, feedback, and sociocultural approaches.
The Agency for Healthcare Research and Quality (AHRQ) supports the Comprehensive Unit-based Safety Program (CUSP), which combines teamwork, communication, and improvements in safety culture with a comprehensive checklist of evidence-based measures aimed at preventing specific HAIs. When the program initially rolled out, then-director of AHRQ Carolyn M. Clancy, MD said:
“Until recently, these infections were thought to be an unfortunate consequence of care. Our work … demonstrates definitively that they are not. These infections can be prevented. These results changed our idea of what’s possible.”
Data shows that since implementing CUSP practices, hospitals cut central line-associated bloodstream infections by 40% – that translates to 2,000 fewer people suffering from infection, and 500 lives saved.
This data is available on PolicyMap and can be found in the Health menu under Hospitals, “Hospitals: Quality of Care”.